The danger of opioids has been a hot topic in the news lately, as pharmaceutical lawsuits and drug overdose deaths are continually rising.
But what led to this increased awareness of opioid addiction? And what makes opioids so dangerous and so addictive?
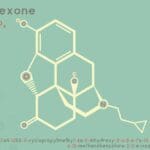
According to The National Alliance of Advocates for Buprenorphine Treatment, opioids are euphoria-inducing drugs and come in natural, synthetic, and semi-synthetic forms. The most natural form of opioids is the endorphins produced in our bodies. Opium is an opioid obtained directly from the opium poppy plant, while morphine and codeine are drugs produced from opium alkaloids. Semi-synthetic opioids include heroin, oxycodone, and buphrenorphine, and there are also fully synthetic drugs, like methadone, that emulate opiates’ effects.
What do opioids do? They “attach to receptors in the brain…Once attached, they send signals to the brain of the ‘opioid effect’ which blocks pain, slows breathing, and has a general calming and anti-depressing effect” (NAABT). The drug’s two-part effect of euphoria and pain blockage covers both bases of recreational or medicinal purposes. Opioid painkillers act as an extension of the endogenous opioid, or endorphin, that is naturally produced. The body’s natural need for endorphins is what can make the brain receptors grow to expect the opioid painkillers after repeated use, as the two types of opioids are indistinguishable to the brain.
One of the reasons that people might abuse an opioid prescription is that its high is different than most misused drugs like alcohol, marijuana or hallucinogens. The high from those drugs is typically accompanied by intoxication or impairment. Opioids, on the other hand, produce “feelings of intense joy and comfort…similar to feelings of great accomplishment, or achievement of a lifetime goal, rather than an impairment” (NAABT).
Opioids have a lengthy history that is filled with both the pros and cons of the drug. According to The Atlantic’s A Brief History of Opioids, opium has been used since 3400 B.C., the first reference being used for its euphoric effects in lower Mesopotamia. In 1806, German chemist Friedrich Serturner introduced morphine, a branch of the opioid family, which became the backbone of American medicine throughout the nineteenth century.
The first recorded wave of American opioid addicts were post-Civil War soldiers that had been treated with morphine; their addiction was then known as the “Soldier’s Disease.” First heroin and then oxycodone were synthesized in an effort to create a safer opioid painkiller than morphine (A Brief History of Opioids).
Medicinal heroin became illegal in 1924, as opioid medications went under the administration of the FDA. Oxycodone was approved in 1950, which sparked the prescription opioid abuse that is still present today. In the 1960s, illegal heroin use rebounded after America’s involvement in Vietnam. In 1970, warnings of the dangers of opioid addiction were thrown into constant circulation due to the Controlled Substance Act, which was shortly followed by President Nixon’s War On Drugs in 1973 (A Brief History of Opioids).
Despite (and possibly in response to) these American efforts to curb the medicinal and recreational opioid use, the World Health Organization (WHO) stated in 1969 that “tolerance and physical dependence did not in itself constitute drug dependence” (A Brief History of Opioids). This claim began to positively influence the general opinion of medicinal opioids.
In 2001, in response to claims that pain was being undertreated, the Joint Commission added a fifth vital sign for doctors to check when treating patients: pain. Making pain an official vital sign placed pressure on doctors to relieve their patients’ discomfort in order to keep up the medicinal reputation of the hospitals that they worked for. The combination of the WHO’s statement, the addition of the fifth vital sign, and some backlash to the previous strict anti-drug movement led to prescription opioids making a significant comeback.
However, as opioid medications have become increasingly common in response to the expectation to treat pain, some questions have started to arise. In April 2016, Medpage Today posted an article, Opioid Crisis: Scrap Pain as 5th Vital Sign?, which argues that pain should be considered only a symptom and not a sign because it cannot be objectively measured as the other four signs can (body temperature, pulse and respiration rate, blood pressure).
Is an opioid medication that is exclusively for medicinal use and does not have possible addictive side-effects a utopian dream? Throughout opioid history, these painkillers have been shuttled between the extremes of being the anchor of medicinal practice, to being the targets of “JUST SAY NO” campaigns. And throughout these extremes and the spectrum in between, opioid painkillers have been both dangerous and beneficial.
So what are we to do? Due to technological and societal developments, we have grown to expect treatment of pain. Opioid medication is an approved, efficient solution, and we have the product. Is the possibility of becoming addicted worth assuaging the pain?
Addiction could be a huge risk to some, yet most people do not even second-guess an opioid prescription. Before taking an opioid painkiller, consider factors like family or personal history of addiction and substance dependency. The bottom line is that opioid painkillers are dangerous when misused or approached indifferently.
It all depends on each person and their situation. Opioid painkillers and medical professionals are not the villains in this story; the villain is the pain. And just like any benefit, relief from pain has a cost. It is up to each person involved—the pharmacist, the doctor, and the patient—to be aware of the cost, and to decide whether it is a chance they are willing to take.
(314) 464-0222. We’re here to help.